Print as PDF
KEY POINTS
- The potentially infectious nature of all blood and body substances necessitates the implementation of infection control practices and policies in the health-care setting.
- The current best-practice guidelines for infection control procedures in Australian health-care settings are outlined in the Australian guidelines for the prevention and control of infection in healthcare (2010) (1).
- The universal application of standard precautions is the minimum level of infection control required in the treatment and care of all patients to prevent transmission of hepatitis B virus (HBV).
- Vaccination is an important infection control strategy for the prevention of HBV. All health-care workers should be vaccinated and be aware of their vaccination and immune status.
- Health-care workers who regularly perform exposure-prone procedures have a responsibility to be regularly tested for human immunodeficiency virus (HIV), hepatitis C virus (HCV) and HBV if they are not immune.
- Hepatitis B infection alone does not disqualify health-care workers with the infection from practice.
- Health-care workers with HBV can perform exposure-prone procedure if their HBV viral load is below 200 IU/mL, provided they have regular, 3 monthly, testing to monitor viral load.
- National Health and Medical Research Council (NHMRC). Australian guidelines for the prevention and control of infection in healthcare (2010). Canberra: Commonwealth of Australia, 2010. Available at: https://www.nhmrc.gov.au/about-us/publications/australian-guidelines-prevention-and-control-infection-healthcare-2019 (last accessed 21 June 2022).
- Redd JT, Baumbach J, Kohn W, Nainan O, Khristova M, Williams I. Patient-to-patient transmission of hepatitis B virus associated with oral surgery. J Infect Dis 2007;195:1311–4.
- Polish LB, Shapiro CN, Bauer F, Klotz P, Ginier P, Roberto RR, et al. Nosocomial transmission of hepatitis B virus associated with the use of a spring-loaded finger-stick device.The New Engl J Med 1992;326:721–5.
- Hutin YJ, Goldstein ST, Varma JK, O’Dair JB, Mast EE, Shapiro CN, et al. An outbreak of hospital-acquired hepatitis B virus infection among patients receiving chronic hemodialysis. Infect Control Hosp Epidemiol 1999;20:731–5.
- Dumpis U, Kovalova Ž, Jansons J, Čupane L, Sominskaya I, Michailova M, et al. An outbreak of HBV and HCV infection in a paediatric oncology ward: epidemiological investigations and prevention of further spread. J Med Virol 2003;69:331–8.
- Samandari T, Malakmadze N, Balter S, Perz JF, Khristova M, Swetnam L, et al. A large outbreak of hepatitis B virus infections associated with frequent injections at a physician’s office. Infect Control Hosp Epidemiol 2005;26:745–50.
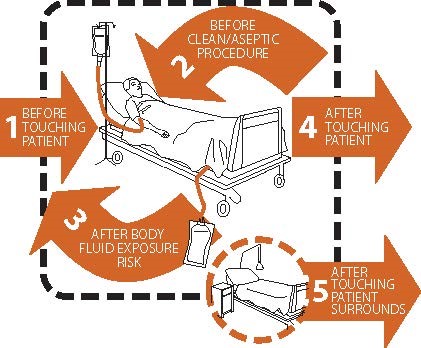
- Sax H, Allegranzi B, Uckay I, Larson E, Boyce J, Pittet D. ‘My five moments for hand hygiene’: a user-centred design approach to understand, train, monitor and report hand hygiene. J Hosp Infect 2007;67: 9–21.
- Ryan K, Havers S, Olsen K, Grayson ML, editors. Hand Hygiene Australia Manual. 5 Moments in Hand Hygiene. 5th edition May 2018. Available at: https://www.hha.org.au/local-implementation/hha-manual (last accessed 4 July 2018).
- Australian Government. Australian Technical Advisory Group on Immunisation (ATAGI). The Australian Immunisation Handbook. Hepatitis B. (updated 2021) [internet]. Canberra: Department of Health; 2018. Available at: https://immunisationhandbook.health.gov.au/contents/vaccine-preventable-diseases/hepatitis-b (last accessed 29 April 2022).
- Communicable Diseases Network Australia (CDNA). Australian national guidelines for the management of health care workers known to be infected with blood-borne viruses. Appendix 1. Canberra: Australian Government. Department of Health and Ageing; 2012. Available at: http://www.health.gov.au/internet/main/publishing.nsf/content/cda-cdna-bloodborne.htm#BBVs (last accessed 4 July 2018).
- Centers for Disease Control and Prevention (CDC). Updated CDC recommendations for the management of hepatitis B virus-infected health-care providers and students. MMWR Recomm Rep 2012;61(RR-3):1–12.
- European Association for the Study of the Liver (EASL). EASL 2017 Clinical Practice Guidelines on the management of hepatitis B virus infection. J Hepatol 2017;67:370–98.
- Royal Australian College of General Practitioners (RACGP). Infection prevention and control standards for general practice and other office-based and community-based practices. 5th edition. 2014. Available at: https://www.racgp.org.au/your-practice/standards/infectioncontrol (last accessed 4 July 2018).